BBC Gets It First, Doctors Get it Right
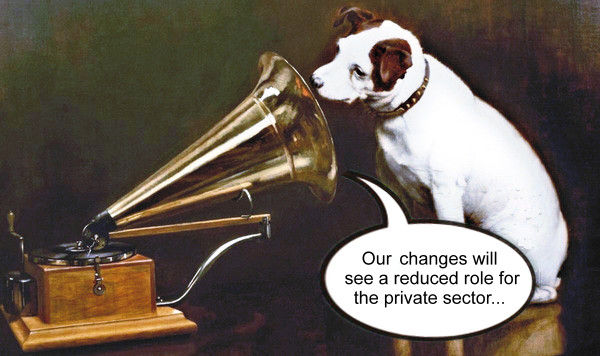
The BBC, now officially the unofficial news station for the Conservative party, came a cropper over the weekend when Hugh Squim, the oleaginous health editor for Broadcasting British Conservatism, reported that a leaked draft NHS white paper proposing radical changes to the NHS ‘would see a reduced role for the private sector’, when in fact it says nothing of the sort. Squim subsequently re-wrote the offending paragraph after being hand-bagged on twitter by the redoubtable Prof P, but the episode only goes to show how sloppy the BBC news reporting has become. It is the BBC’s job to give us unbiased fact based news, not our job to correct it’s shoddy reporting with the true facts. What can we glean from the leaked draft?
The first hurdle to be overcome is the writing style, which is that of a brainwashed second rate intern with a buzz word fetish. The draft shows exemplary inclusivity and diversity: all last year’s words are there, from organisational silos to collaborative working in an agile framework, all threaded on a turgid syntax, up with which we should not have to put. This is further padded out with a lot of sanctimonious hogwash about learning lessons from how well the NHS responded to the coronavirus pandemic. This fatuous clappery, like the Thursday evening ritual last spring, rather ignores the fact that much of the response, which ranged from pretty much shutting down elective care, to dumping any patient fit enough to be strapped to a trolley on a beleaguered care sector, not to mention the Department of Health and Social Care’s hideous frenzy to blow billions on failed contracts with the private sector, hardly covered the NHS, let alone the Department, in shining glory.
That much at least is history. What does the draft white paper have to say about the future? On a first reading, once one has managed an agile exit from the organised silo of Whitehall hogwash, several themes emerge, none of them encouraging. The big one is a move to integrated care, which this post will cover, but there are significant others that will have to wait for another day. These include, among other things, a power grab by ministers (‘we want to strengthen the Secretary of State’s powers of intervention, oversight and direction [over NHS England, a new merged over-arching body]’), plans to create a charter for coercive healthism (‘care that focuses not just on treating particular conditions, but also on lifestyles, on healthy behaviours and prevention’), and, alongside that, plans to encourage an orgy of data sharing (‘[we] will set out a range of proposals to address cultural, behavioural and legislative barriers to data sharing’ that will in time allow care to be ‘informed by a better data drive…identifying those who are at risk and who we can impact…’). Cripes.
But, for now, back to integrated care. It sounds like a wonderful thing, but it is in fact a euphemism for managed care, a heinously rigid form of healthcare delivery much favoured by that country notorious for its outrageously expensive yet remarkably ineffective healthcare, given the enormous outlay, the United States of America. OECD data repeatedly shows America as the highest per capita spending on healthcare country in the world (play around with the sliders on the OECD chart to get the historical picture), and yet its health outcomes, measured by current life expectancy both at birth and at age 65, is mediocre, and on both measures is worse than the United Kingdom (again, Dr No recommends playing around with the settings and sliders on the OECD charts to get the full picture).
A fundamental problem with American healthcare is that it is largely private, and so is as largely concerned with the profit motive as it is with providing healthcare; and healthcare does not work well when it has to serve two masters. Many decades ago, we in the United Kingdom had the good sense to realise that the only sensible way to fund and run a health service is to have a publicly owned and provided service paid for out of taxation. Most, but not all, with America the standout exception, developed countries have come to much the same conclusion, albeit in many cases with a bastardised private-public healthcare system.
Managed care, on the other hand, as developed and implemented in the United States, is a for-profit insurance based system, with the ‘managed’ care, provided by so called health maintenance organisations, or HMOs, a crude but, as the OECD data shows, failed attempt to contain costs. But at the same time, ‘management’ rigorously controls what can and can’t be done by individual doctors; and so, in the land of the free, they find themselves paying more for less. Choice, that evil chimera in the land of healthcare, is an illusion for most Americans; instead, it is the invisible hand not of the market, but of the accountant, that decides what treatment they will or will not get.
The draft white paper, if it becomes law, will set up a similar management structure here. It will do away with CCGs (the GP based system for commissioning healthcare) and all the competitive purchaser provider split paraphernalia, and replace the whole lot with ‘integrated care systems’. We want, says the draft white paper, ‘to legislate for every part of England to be covered by an integrated care system (ICS)’. There is much waffle about duties to collaborate — about as hopeful as locking two tom cats in a room and ordering them to collaborate — but make no mistake, these ‘integrated care systems’ are boilerplate HMOs, to be imposed on the NHS. If the draft white paper ever makes it into law, then we too, like America, will have managed care, rigorously and tightly controlled by HMOs dressed as integrated care systems.
Far from ‘seeing a reduced role for the private sector’, the private sector will have direct access to the NHS, unfettered by tiresome competition rules. ‘We anticipate that there will continue to be an important role for voluntary and independent sector providers,’ the draft says, ‘but we want to ensure that where there is no value is running a competitive procurement process that services can be arranged with the most appropriate provider’. No need to bother with all that competition nonsense round here. Instead, private interests will become partners, not only let in through the back door as services are ‘arranged with the most appropriate provider’, but also welcomed with open arms at the front door, as members of new ICS Health and Care Partnerships, with members drawn from a wide range of ‘partner organisations’ including ‘voluntary and independent sector partners’, and ‘tasked with promoting partnership arrangements’. Or, to put that partnership word salad into plain English, the private sector will have a seat at the NHS table where it can promote its own interests.
If all this seems fanciful, recall what has happened over the last year. NHS contacts worth billions of pounds of tax payers money have been awarded without competitive tender to private concerns. Then the draft white paper starts to make a whole lot more sense: it is merely the first draft of a bill to enact what has already started to take place.

Is private healthcare
?
Not so: when the money flows from the customer or patient to the hospital and clinicians there is only a single master, the customer. This is not to defend the US healthcare system of which I have no experience but the German system of Krankenkassen gives the individual considerable control of where and how he is treated.
Why is it that defenders of the NHS always argue that the US system is the only alternative to what we have in the UK when there are other models that work better?
‘… , and yet its health outcomes, measured by current life expectancy both at birth and at age 65, is mediocre, ‘
That’s because so many young men in ‘the hood’ shoot each other, and it has large scale influx of immigrants from impoverished southern Countries who live in bad conditions mostly outside the system.
Having worked for a US healthcare company for 25 years, and consequently with experience of European healthcare, I can attest US healthcare is second to none.
‘ A fundamental problem with American healthcare is that it is largely private, and so is as largely concerned with the profit motive as it is with providing healthcare; and healthcare does not work well when it has to serve two masters.’
This is not so.
Medicaid for those on low-incomes, and Medicare subsidised cover for the elderly are Federal programmes which have been extended more and more over the years. On top of these, each State has its own schemes for those not covered by private insurance.
That dog’s breakfast, The Affordable Healthcare Bill aka Obamacare, makes it a Federal Offence not to buy health insurance, punishable by fines. For a number of reasons this has driven the cost of private insurance up. Many now unable to afford it, are enrolled in Medicaid.
In fact the US healthcare is largely Government, and that is the problem now.
If I could chose where to get ill it would be the USA.
Dr Theodore Dalrymple has something germane to say today.
“Bureaucracy and the Tin-Pot Stasi”
https://lawliberty.org/bureaucracy-and-the-tin-pot-stasi/
The first paragraph, while addressing the British criminal justice system, applies equally to the NHS.
“A pure bureaucracy, which is what the British criminal justice system has become in all but name, will do almost anything rather than solve the problem with which it is presented. It will invent any number of complex procedures ostensibly meant to solve a problem, but really just designed to keep itself busy. A problem solved, after all, poses a potential threat to a bureaucracy, insofar as it might be used to justify a reduction in its size whenever the next round of budgetary cuts is proposed”.
I think it is a fundamental mistake to argue about whether medicine should be publicly or privately owned.
It’s the scale at which things are done that matters far more. Public or private, the scope for selfishness and greed is just as great – as many of us discovered to our dismay when Mrs Thatcher replaced the dead hand of the trade unions with the King Stork of big business.
As Mr Hodge observes, the NHS and the US “system” are not the only models. The French medical system, from what I have seen of it, seems to work rather better than either.
And what is so wrong with what we had before the NHS? A mixture of big and small, run on many different lines, and giving plenty of scope for competition and different approaches.
But even the NHS might work well if we could somehow get rid of all the “management” and “administrative” deadwood that soaks up most of the money, one way or another.
As one of Scott Adams’ marvellous “Dilbert” books is entitled, “Don’t Step in the Management”.
“the only sensible way to fund and run a health service is to have a publicly owned and provided service paid for out of taxation.”
The Germans know better. I must say I’m weary of the endless attempts to use the US “system” as a bogey-man. I’ve never met anyone in my life who has wanted to introduce the US system here.
The Labour Party has been running this absurd scare story since -what? – the 80s; certainly the early 90s. Privatise, American, Ronald Reagan, Privatise, American, Donald Trump. Chuck it, Dr No. You are keeping low company.
Dr No thought he might get some flak for this post. It is not one of his best, because, apart from anything else, it breaks one of his cardinal rules, though like all rules it gets broken from time to time: one post, one topic. So he deserves flak for his drive by shooting at the American healthcare system (it’s always America because it’s an easy target, given the OECD, or similar, figures) and pot shots at the chimera of choice. These are parts of much more complex debates (how do you decide what makes a good health care system, and who if anyone has achieved that? what is the role of choice and competition in healthcare? etc) and so really should have posts of their own. Dr No is not dodging them, anything but, just suggesting instead that they deserve fuller discussion in their own right.
The ‘one topic’ for this ‘one post’ is the clues revealed by an early draft of a white paper (so it may change substantially, or even never happen) about the likely direction the government wants the NHS to take, with the obvious main themes gleaned from a first reading of the draft listed in paragraph three of the post. Of these, despite its dull sounding name, the move towards integrated care struck Dr No as the most significant, all the more so because of the way it is to be implemented. This includes the move to allow the private sector to join the new ‘ICS health and care Partnerships’ that will influence ‘ICS NHS bodies’ (sorry, the jargon’s from the draft) who in turn will arrange for services ‘with the most appropriate provider’. If this isn’t a recipe for conflicts of interest, Dr No doesn’t know what is! Then add in the actual behaviour we have seen during the pandemic (billions going to private concerns with little or no tendering), and the reliance the draft places on ‘learning’ from the pandemic, and Dr No for one can see that the over-used phrase ‘what could possibly go wrong’ might have a place here.
“…how do you decide what makes a good health care system…?”
That seems to me to be exactly the right question. And I think that, like all really good questions, as soon as it is asked it illuminates much of what is wrong with the existing system.
A good health care system, of course, has as its primary focus the welfare of patients – even to the extent of helping them to stay healthy and thus not become sick in the first place.
How is that done? Start with doctors, nurses, radiologists and other specialists, add porters, cleaners, etc.; give them suitable premises and equipment.
When designing such a system, surely administration and management come way down the line. As far as possible, everything should be designed by the experts who do the work: doctors, nurses, etc.
Gigantic schemes of finance, computerisation, etc. seem very low priorities; and if most surgeries, clinics and hospitals are of moderate size, their own people should be able to do most of the organisation in their spare time. (Given enough staff to begin with).
The chief objection to the American system is surely that it inverts the proper priorities, putting the making of money first and foremost, closely followed by the evasion of accountability.
Long ago I had an unusually intelligent GP. One day, to my surprise, he raised the subject of the reforms that had just been introduced by the Conservatives – John Major’s government, maybe? Anyway he moaned about them. Oh he moaned.
Some years later he raised the subject of the scrapping of those reforms by Labour. Oh how he missed the Conservatives’ system. It had been far better. His earlier moaning had been quite wrong-headed.
Conclusion: I pay no heed to doctors’ prognostications about recent, or proposed, reforms.
I also remember a long ago dinner party where the subject turned to the NHS. Everyone who had lived abroad said they’d used a better system there. The conversation was capped by a woman who avowed the superiority of her experiences in France, the Netherlands, Canada, and ICELAND!
Still there are people who claim to believe that the NHS is the envy of the world while being at a loss to explain why nobody in the world has copied it.
Conclusion: it’s a system so bad that nobody would reimpose it today. How to wriggle out of it and introduce something better is an irrelevant question. You can’t expunge an Established Religion by Act of Parliament. At least not nowadays. Whether you can even reform it for the better is doubtful. I’ll believe that it’s been improved when the hospitals achieve even a modest competence at infection control.
Tom – exactly. Dr No qualified in 1982, in a very different world, where senior doctors and nurses ran the show. It was a world far closer to Sir Lancelot Spratt’s world than today’s world. At some point, Dr No will probably do a post on this (as part of what makes a good health service, perhaps). As he said in the earlier comment, this particular original post was overloaded with too many topics, but these comments are useful reminder he needs to get round to doing these other posts.
dearieme – Dr No has been known to say prognosis is piece of string whose length is not known until it is cut, and the same uncertainties we may be sure apply to other prognostications. But that doesn’t mean we shouldn’t make prognostications, medical or otherwise.
The changes you refer to in your first paragraph are almost certainly the 1990 New Contract for GPs, brought in right at the end of the Thatcher years. A few years earlier Ken Clark had signalled Tory intents by referring the health service as an industry (it’s not, the clue is in the name, and like the other big one(s) with service in the name, the Armed Services, and both exist to provide a service, not to make money, though both of course spawn very lucrative industries, arms and pharma). Clark also introduced the idea of the purchaser-provider split.
Dr No was doing his GP trainee year at the time the New Contract appeared. It was radical enough to put Dr No off a formal career in general practice, so wide-ranging (and unpalatable to GPs) were the changes. The chief one that we objected to the most was interference in our weekly round on the golf course (there is. by the way, a serious point in there, about control, and since the golf was played against the local consultants, a useful time could be had by all).
Interestingly Prof P tweeted a link today to news that the UK arm of a pretty large American owned managed care corporation, Centene Corporation, is to take over 49 surgeries in London to add to its existing portfolio of 20 or so facilities. Perhaps the real question isn’t about whether the Americans are invading the NHS, but how fast they are invading the NHS. It also appears Centene has a ‘significant influence’, but not a controlling one, over Circle Health, who you may recall were the oufit behind the Hinchingbrooke Hospital shenanigans.
The White paper has now been published. As far as Dr No can see, the key phrasings remain unchanged from the draft version. Depressingly, Squim was on the Today programme this morning, once again back to echoing his master’s voice.
Dr
If we were to form a wide (experience, including non medics) but not too large panel to discuss the best health care system in the world currently. What odds would you give that the NHS or the US version would make the top 10? It seems to me that the NHS is too large and cumbersome and resistant to change, it also holds the positions of political football (and propaganda tool) and public sacred cow. The US leaves many behind and care in its widest sense is not always the priority of the system. Whilst I agree to apportion blame in healthcare is a slippery slope to be avoided and public health declarations are often seriously flawed, nutrition advice is a classic example of the blind leading the clueless, how do we get people to understand the limited resources available? Could a small charge (with a yearly cap), like Sweden, instil a sense of personal investment in healthcare that is hidden with taxation currently?
Although I have no expertise and little experience, I think that France and Russia might be near the top. Stories I have heard about Russian health care (mostly from US visitors) make it sound attractive. Rapid attention, skilful diagnosis and treatment, concern for the individual patient, and extremely low charges.
Rick + Tom – the first thing to consider is the criteria used to rank healthcare systems, and they can very very widely. For example, the OECD data linked to in the OP on their own say the USA is pretty dreadful, hugely expensive, with only mediocre life expectancy outcomes (and on both measures scores worse than the NHS). But on other things (local excellence, if you have insurance and are in the right place at the right time) it can do very well. So it is really back to the ‘what makes a good health care system’ as the starting point; then you can assess how different systems measure up.
DN has never favoured the small co-payment charge, because it would hit those who need to access healthcare the hardest (inverse care law). The well off worried well would still turn up, and probably start acting out entitlement to boot, while the single mum on the breadline would decide not to get an appt because she couldn’t afford it. Yes, Dr No knows there are many who abuse the system, but the thing is you tolerate them (and try to persuade them to use the NHS better) so the one who does need to be seen can be seen. It’s not socialist medicine, it’s humane medicine.
Homework for anyone who fancies it: compare and contrast hysterectomy rates in the UK and the USA.
I skimmed through the White Paper the other night. Dr No has summarised drafting style with painful accuracy. As soon as I came across the commitment to avoid a ‘one size fits all’ approach, I knew that it had been drafted by someone with a 3rd rate intellect who had learned their craft in the New Labour era of bureaucratic crap-speak. It got worse after that.
Fascinating, Dr No, et al, thank you.
Yes: ‘It’s not socialist medicine, it’s humane medicine’, for all sorts of reasons.
Hippocentaurus, put very succinctly!
My view is pretty basic; I am sad the public is being lied to to a level which beggar’s belief. I am sad for the millions of Mr and Mrs Blogs who are desperately trying, on endless insistence and promise, to ‘save our NHS’, which isn’t ‘ours’ at all any more, and which is continuing to systematically being demolished by the very people insisting on the ‘saving of it’ by us, and through all the ridiculous measures we continue to suffer. Whether the NHS is a good system (any more) compared to elsewhere, or whether it isn’t, the fact that Jo Blogs has no idea what’s really going on is absolutely appalling. That he claps those working under many of the the pseudo blue & white banners in his local hospital, whilst being encouraged to go on thinking it’s really ‘the (or even ‘his’) NHS’, is shocking. I suppose the truth might out one day….. Poor Mr and Mrs Blogs.