Mask Wars

The biggest fact about face masks and covid–19 is there are no facts. This should not surprise us one bit. Covid–19 is a new disease, and research takes time to conduct. Furthermore, the sort of research that would give us a definitive answer, a randomised controlled trial, is burdened with almost — but not totally — insurmountable difficulties, from ethical concerns to procedural obstacles. One solution, attempted by the three authors of the Royal Society report covered by Dr No in his last post, is not to let the best be the enemy of the good, a pragmatic wheeze that says that the absence of the great (RCT evidence) doesn’t mean we should ignore the good (lower quality but, one hopes, tolerable evidence). The danger is that following Voltaire can all to easily turn into ‘no need to bother with that sort of nonsense round here’, where ‘that sort of nonsense’ is good quality evidence. This is what the Royal Society report authors did. Having found no reliable clinical evidence, they turned instead to an in vitro, laboratory based physics experiment, and came to a clinical conclusion. Dr No regrets to say that simply won’t wash. But then again, you hire demographers, you get pyramids.
Official policies on the wearing of face mask to reduce covid–19 transmission have followed a curious trajectories. For WHO, according to Newsnight, it was a case of when the political winds change, we scientists change our minds — science led by the politics, rather than the other way round. Much the same horse-cart reversal seems to have happened at the Royal Society. In Westminster, masks were decried for months, debated for days, and then ordered in hours: face masks are to be compulsory in English shops from the 24th July. Missing from this ordinance is any explanation as to why masks only become effective on the 24th — presumably, if they work on the 24th, they should also work on the 23rd, and every other day from now up until the 24th. Even more curious than the trajectories is the universal lack of robust evidence underpinning the policy decisions.
There is no shortage of quoted research, but when examined, it is invariably found wanting. This should come as no surprise to readers of Bad Medicine: references used in research papers to back up assertions are rarely checked by casual readers. When they are checked, it often turns out that creative referencing, a close cousin of creative accounting, is at work. A widely quoted Lancet paper, for example, concluded that ‘face mask use could result in a large reduction in risk of infection’, but this albeit conditional assertion is based numerous studies in a variety of settings using different types of masks. If we zoom in on the studies that cover non-healthcare ie community face mask use, the hundreds of studies in dozens of countries involving tens of thousands of subjects dwindles to just three studies in two countries involving some 725 patients (if that – the numbers are not transparent). None of the three studies looked at covid–19 transmission (they were about SARS), all three were retrospective, and not one was designed with the specific intention of assessing mask effectiveness per se. Let us zoom in even closer on the three studies, seen here on the Lancet Forest plot:
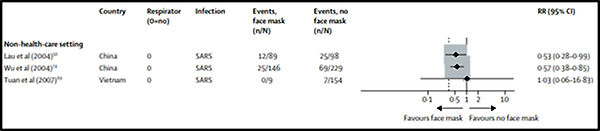
Trimmed snapshot from Figure 4: Forest plot showing unadjusted estimates for the association of face mask use with viral infection from Chu et al (2020) (link to paper in paragraph above).
Lau et al (2004) investigated ‘Probable Secondary Infections in Households of SARS Patients in Hong Kong’. It is not clear where in this study the Lancet authors got their numbers from, but it doesn’t really matter because this isn’t a community study of masks, given the data collected was on mask usage when visiting patients in hospital. A hospital is not a ‘non-health-care setting’. One paper down, two to go.
Wu et al (2004) investigated ‘Risk Factors for SARS among Persons without Known Contact with SARS Patients, Beijing, China’. This turns out to be a small case-control study of just under 100 self-selected (50% of those contacted refused to take part) cases (again, the source of the Lancet numbers is not apparent in this paper) that did find mask wearing was protective for the wearer, and this was ‘dose dependent’ — always wearing a mask was more effective than sometimes wearing a mask. This weak small number of cases case-control study might provide a tiny crumb of comfort to the pro-mask brigade were it not for the fact that it only looked at wearer protection, and so tells us nothing about protection for others. But that is not the killer blow, which is to be found in one brief sentence in the Definitions section: ‘Laboratory testing for SARS-CoV was not part of the case definition’. Instead, cases were defined on a combined clinical and ‘there’s a lot of it about’ basis (Dr No kids you not — read the paper), but, as it turns out, there wasn’t a lot of it about: of the 31 blood tests that were done, only 8 (26%) came back positive. The whole paper is a meaningless chimera. Two papers down, one to go.
Tuan et al (2007) (actually, it’s 2006, but what’s a year between friends) investigated ‘SARS transmission in Vietnam outside of the health-care setting’. That this paper should be presented as evidence that face masks protect the wearer is a long long way south of bizarre. Of 9 (that’s right, nine) subjects who reported ‘sometimes/most times’ wearing a mask ‘during contact with case’, none got infected, while 7 of 147 non-maskers did get infected, yielding a quoted odds ratio of 0 (CI 0–15.37, p value = 1). For non-statistical readers, an odds ratio of 0, a confidence interval ranging from 0 to 15.37 and a p value of 1 mean just one thing: don’t touch this result with a barge pole. Three papers down, none to go.
And so on. The evidence that face masks work simply is not there, for the reasons Dr No outlined right at the start of this post. There does appear to be one isolated pre-covid–19 cluster based RCT looking at cloth masks compared with medical masks in healthcare workers, but it is often discounted, reasonably enough, on the grounds that the control group was contaminated (some of the ‘controls’ wore masks anyway). Furthermore, it is not community based, and only looked at wearer protection. Nonetheless, flaws (and they are significant) notwithstanding, the research found that ‘the rates of all infection outcomes were highest in the cloth mask arm’ and concluded ‘this study is the first RCT of cloth masks, and the results caution against the use of cloth masks‘. There are a myriad other concerns about masks, from their deleterious effects on human interaction, to their induction of ill-advised covid–19 complacency in wearers. In short, the ‘evidence’ swings both ways. Just as masks might be beneficial, so too might they be harmful.
The ongoing scientific uncertainty is fertile ground for twitter wars, and sure enough the twitterati are hard at it. Facts, or rather the absence of facts, counts for nothing. One widely used ‘once more for the people who don’t get it’ image claiming to be based on John Hopkins research shows bilateral mask wearing reduces transmission to 1.5%, from 70% for no mask wearing. There is no such John Hopkins research. If the misinformation, aggression and downright thuggery so evident on twitter spills out even in only a fraction onto the streets as the 24th July approaches, the police aren’t going have time to worry about mask refuseniks. They are going to have more than their hands full separating the warring factions, and will conclude, if they haven’t already done so, that making mask wearing compulsory in shops was about as dumb as dumb gets.

Muzzles visible in public spaces, or specifically shops, serves the government well; in that it stirs up people’s emotions — to be forever ‘frit’ of the invisible killer whilst rejecting the notion that the politicians panicked and got it all wrong! So the sheep won’t ask subversive questions in a climate of fear and control.
Common sense, and less invasive practices should prevail — washing hands, losing weight, boosting your immune system. Nor will it condemn the shops in an already tanked economy.
Have you seen Leung, Chen et al (2020)?
John – Not sure I can positively identify the reference. The only thing I could find that seemed to match was a short letter in the Lancet from March (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7133583/pdf/main.pdf) summarising a number of the pro mask arguments but not containing any new evidence. Do you by any chance have a doi for the reference?
Edit: that letter is Leung and Cheng, not Leung and Chen, so it probably isn’t the correct reference.
The difficulty is that all the studies to date (for the reasons given in the first paragraph of the post: covid-19 is new, and proper trials are difficult but not impossible to do) are in some shape or form proxy studies, in that they show something that isn’t reduced transmission, but may be relevant, and then extrapolate to say that nonetheless transmission will/may be reduced. As in statin studies, they are mistaking the finger (cholesterol) pointing at the moon for the moon (cardiovascular disease) and as the statin studies demonstrated, the finger doesn’t always point at the moon.
There’s another study worth mentioning: the Edinburgh mask study. The press release (https://www.ed.ac.uk/covid-19-response/latest-news/face-coverings-covid-19-transmission-risk) title clains ‘Face coverings can reduce Covid-19 transmission risk’ – note the can rather than do – but lower down it says ‘Surgical masks and the tested hand-made masks were found to limit the forward flow of a breath out, but also generate far-reaching leakage jets to the side, behind, above and below. Heavy breathing and coughing, in particular, were shown to generate intense backward jets’. Intense backward jets…woe betide anyone on the bus sitting behind someone wearing such a mask…
The full preprint is here: https://arxiv.org/ftp/arxiv/papers/2005/2005.10720.pdf. For those who appreciate visual information, some of the images of the effects of mask wearing are particularly telling. Section 3.3 Different Leakage Types also makes for ‘interesting’ reading.